CIC Exam Dumps - CBIC Certified Infection Control Exam
Searching for workable clues to ace the CBIC CIC Exam? You’re on the right place! ExamCert has realistic, trusted and authentic exam prep tools to help you achieve your desired credential. ExamCert’s CIC PDF Study Guide, Testing Engine and Exam Dumps follow a reliable exam preparation strategy, providing you the most relevant and updated study material that is crafted in an easy to learn format of questions and answers. ExamCert’s study tools aim at simplifying all complex and confusing concepts of the exam and introduce you to the real exam scenario and practice it with the help of its testing engine and real exam dumps
Which of the following statements describes the MOST important consideration of an infection preventionist when assessing the effectiveness of an infection control action plan?
A nutrition support team wants to determine whether patients who receive total parenteral nutrition (TPN) at home are at increased risk of central line–associated bloodstream infection (CLABSI) compared with patients who receive TPN in the hospital. The BEST way to compare these two groups is to calculate the:
The expectation to call out or speak up when an infection prevention lapse is observed is an example of
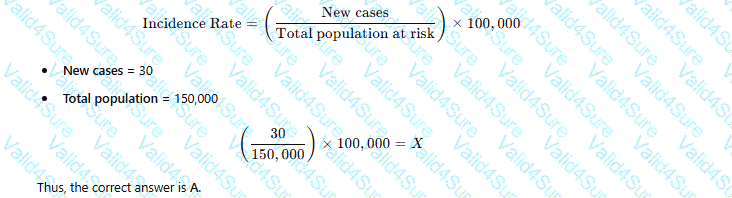
A city has a population of 150.000. Thirty new cases of tuberculosis (TB) were diagnosed in the city last year. These now cases brought the total number of active TB cases in the city last year to 115. Which of the following equations represents the incidence rate tor TB per 100.000 in that year?
An infection preventionist has decided to perform surveillance for central line–associated bloodstream infections (CLABSIs) in the facility’s ICU. Which of the following is the MOST appropriate denominator to calculate risk-adjusted rates?
A 17-year-old presents to the Emergency Department with fever, stiff neck, and vomiting. A lumbar puncture is done. The Gram stain shows Gram negative diplocooci. Presumptive identification of the organism is
The BEST roommate selection for a patient with active shingles would be a patient who has had
A healthcare professional in a clinical microbiology laboratory is concerned about routine exposure to Neisseria meningitidis in culture. The healthcare professional last received the Meningococcal vaccine 8 years ago. What recommendation should be given to the healthcare professional regarding their meningococcal vaccination?